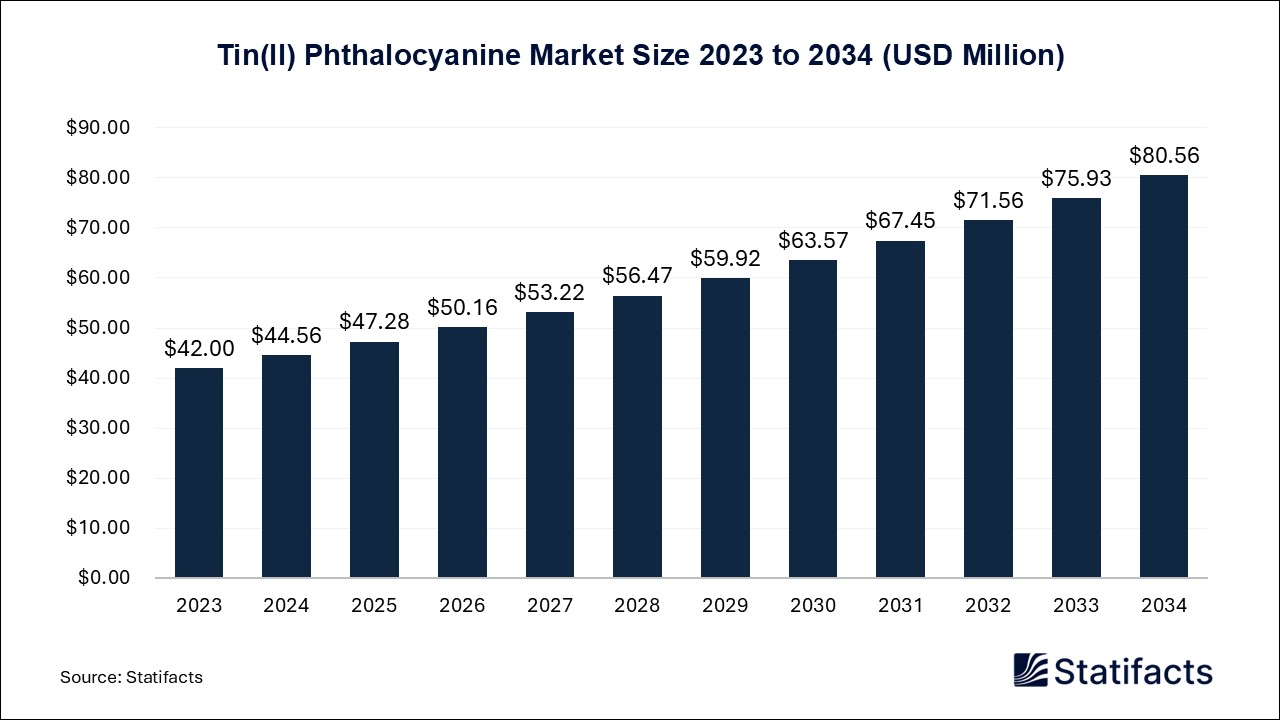
Last Updated: 01 Aug 2025
Source: Statifacts
By clicking “Accept All Cookies” you agree to the storing of cookies on your device to enhance site navigation, analyze site usage, and assist in our marketing efforts.
Privacy PolicySystemic Radiotherapy Market (By Application Area: Hematological Malignancies, Solid Tumors; By End-User: Hospitals, Research Institutes, Outpatient Clinics, Diagnostic Centers; By Mechanism of Action: Direct Cell Targeting, Targeted Gene Delivery, Combination Therapies; By Therapeutic Purpose: Palliative Care, Curing Cancer, Adjuvant Treatment, Salvage Therapy; By Region: North America, Europe, Asia Pacific, Latin America, Middle East and Africa) Industry Size, Share, Growth, Trends 2025 to 2034.
The global systemic radiotherapy market size accounted for USD 5.22 billion in 2024 and is predicted to touch around USD 10.86 billion by 2034, growing at a CAGR of 7.60% from 2025 to 2034. The global market is expected to expand, driven by the growing number of cancer patients. Recent data suggest the demand is particularly high for metastatic cancers that require systemic targeted treatment. Ongoing improvements in radiopharmaceuticals and radioisotope production, especially with the development of newer alpha and beta-emitting agents, continue to provide innovation in this space.
| Reports Attributes | Statistics |
| Market Size in 2024 | USD 5.22 Billion |
| Market Size in 2025 | USD 5.62 Billion |
| Market Size in 2031 | USD 8.72 Billion |
| Market Size by 2034 | USD 10.86 Billion |
| CAGR 2025 to 2034 | 7.60% |
| Base Year | 2024 |
| Forecast Period | 2025 to 2034 |
Systemic radiotherapy uses internal radiation therapy, where drugs with radioactivity or radiopharmaceuticals are given orally or through an IV, to treat cancer by targeting the cancer cells inside the body. Systemic methods have become an effective therapeutic option for many cancers, especially for metastatic cancers, including cancer lines originating from thyroid, prostate, or neuroendocrine, where conventional localized radiotherapy is not sufficient. Systemic radiotherapy has been rapidly acquired by cancer care departments (i.e., oncology, nuclear medicine) and specialized cancer care centers within hospitals, since they can effectively use radiopharmaceuticals for cancer therapeutics. The therapy has potential for several sectors, including hospitals, diagnostic imaging centers, and biopharmaceutical businesses that are developing oncology drugs.
The systemic radiotherapy market outlook appears to be expanding with increasing demand for theranostics, where both imaging and therapeutic uses of the same radiopharmaceutical compound can be performed. Put simply, there is a growing awareness and interest in process development involving systemic radiotherapy. However, the market is also presenting possibilities for alternative therapeutic innovations such as targeted alpha therapy (TAT), beta-emitting radiopharmaceuticals, increased availability of radioisotopes due to government support, and a growing senior population increased incidence of radio-sensitive cancers, which is driving the clinical use of systemic radiotherapy within both developed and emergent care market segments.
AI has been increasingly adopted into systemic radiotherapy and theranostics, increasing operator efficiency and personalizing the treatment path. AI-based systems utilizing automation help automate image segmentation, organ and tumor contouring, and quantitative image measurements, thereby improving dosimetry usage for patient-specific radiopharmaceutical therapies. AI systems limit inter-operator variability when planning the dose and help automate the segmentation and registration of PET/SPECT images for determining the absorbed dose to the patient, while accounting for their specific kinetics. Furthermore, AI aids in hospital-based workflow optimizations within the nuclear medicine department, for example, by automating scheduling, screening for patient risk, and scanner quality control and protocol, leaving technologists free to spend more time on treating their patients and improving throughput. In March of 2024, RefleXion Medical allied with Limbus AI to integrate Limbus Contour into the RefleXion X1 planning system.
The market trends in the systemic radiotherapy market are driven by the rising adoption of theranostics and targeted radiopharmaceutical therapies, as well as advanced radiochemistry, infrastructure investments, and AI-enabled dosimetry.
Rising adoption of theranostics and targeted radiopharmaceutical therapies
The primary driver of growth is the emergence of theranostic approaches that combine diagnostics with targeted radiotherapy. New theranostic personalized therapies are emerging that will ultimately treat metastatic prostate cancer and neuroendocrine tumors in combination with systemically administered, oncologic radiotherapy specifically (but not limited to) novel PSMA- and somatostatin-receptor targeted treatments utilizing lutetium 177 and actinium 225 radiopharmaceuticals. The increasing clinical acceptance of systemic radiotherapy is being deeply enhanced by the industry momentum and, in particular, the prospects of ongoing Phase I/II clinical studies of actinium 225 PSMA-R2 and NeoBOMB1 in breast and prostate cancer indications. The expansion of the theranostic pipeline and, in tandem with regulatory expansion (for example, the FDA expanded the indication of Lu PSMA 617 for use in March 2025), will help to fuel the emergent demands outlined above.
Advanced radiochemistry, infrastructure investments, and AI-enabled dosimetry
A significant driver in the systemic radiotherapy market is the accelerating pace of progress in isotope production, manufacture infrastructure, and AI-enabled dosimetry platforms. In recent times, automated synthesis systems and advances in cyclotron and reactor-based production of isotopes have dramatically improved the availability of important radionuclides, such as actinium-225, gallium-68, and lutetium-177, increasing throughput for radiopharmaceutical supply chains. At the same time, AI-based dosimetry solutions and systems from Siemens Healthineers, GE Healthcare, Mirada Medical, and MIM Software have accelerated segmentation for tissue and organs, time-activity curve fitting, and absorbed dose calculations, thereby further improving precision and minimizing variability across clinics.
As a minor driver of the industry, growing public and private investments in nuclear medicine infrastructure, including regulations, and the growth of facilities, especially in emerging markets, will expand access to systemic radiotherapy services to new patient populations. In 2025, Siemens Healthineers introduced AI-based PET/CT dosimetry tools for automated lesion segmentation and quantification that directly support more accurate patient-specific dose planning associated with broader clinical use.
Key restraints holding back the systemic radiotherapy market include regulatory and validation challenges in AI and radiopharmaceutical implementation, and workforce and implementation barriers affecting AI adoption.
Regulatory and validation challenges in AI and radiopharmaceutical implementation
One major constraint of the systemic radiotherapy market is the complicated regulatory landscape, as well as the considerable clinical validation needed for new AI-enabled tools and radiopharmaceutical therapies. Regulatory bodies are very slowly streamlining application pathways for approvals of radiopharmaceuticals, and AI-based dosimetry and treatment-planning systems need multicenter validation plus an integration into guidelines, before they will be widely accepted in the clinic.
Additionally, professional societies and academic organizations are placing strong emphasis on the need to develop standard validation processes for AI in nuclear medicine so that implementation is postponed until sufficient validation is completed. For example, in early 2025, experts raised the importance of multicenter, multigroup validation studies of AI-enabled dosimetry, wherein many of these studies needed to meet international guidelines before regular adoption for clinical application in radiopharmaceutical therapy, as validation was identified as a limiting factor in pace.
Workforce and implementation barriers affecting AI adoption
A key barrier to adoption is concerns about workforce readiness in implementing AI technology and overcoming barriers to infrastructure change. For instance, there are AI tools, such as auto-contouring and workflow automation, which make processes more efficient. However, organizations, especially those in the UK, have faced obstacles with ongoing funding cuts to resource provisions, staff shortages, and organizational inefficiencies in implementing technology. Suppose there are no ready and available training opportunities. In that case, there are questions regarding the ability of clinical staff to manage AI-driven quality-control systems and how to safely incorporate them into nuclear medicine workflows, which raises unanswered questions about the feasibility of sustainable adoption and clinical alignment.
Another possibility is future clinical expansion of promising radiopharmaceutical agents and indications such as actinium-225-PSMA-R2 and NeoBOMB1 in a variety of cancers, notably prostate and breast cancer. The expansion in the clinical indications is to take place in 2025 with the completion of current phase I/II trials of 225Ac-PSMA-R2 in patients with metastatic prostate cancer and 177Lu-NeoBOMB1 in GRPR-positive patients with breast cancer.
Regulatory timelines drive the movement ahead in clinical development. The FDA has already expanded Lu-PSMA-617's indication in March 2025, and this may be followed by even more label expansions and additional agents. The regulatory movements, particularly in the US, will ultimately drive clinical uptake and even more markets beyond traditional oncology centers globally for treating metastatic cancers that lack existing systemic radiotherapy options.
"This is an exciting step towards identifying alternative treatments outside of frontline systemic therapy. "In select patients, this treatment will result in less toxicities, health care expenditures, and visits to the doctor, without compromising cancer control."
“For a fraction of lung cancers where we aren’t expecting therapy responses, radiation may be particularly effective to help circumvent primary resistance to immunotherapy; this could potentially apply to acquired resistance, too.”
Why Is Lobenguane (I-131) Leading Systemic Radiotherapy Growth?
The Lobenguane (I-131) segment dominated and is anticipated to be the fastest growing segment in the market, primarily due to its general acceptance as an effective treatment for neuroendocrine tumors and pheochromocytoma/paraganglioma tumors requiring systemic targeting. I-131-labeled metaiodobenzylguanidine (MIBG) does have a strong safety and efficacy relationship and is often hailed as a benchmark therapy, but predominately the strength of its clinical use and established acceptance for reimbursement purposes.
The Samarium-153 segment is anticipated to show a notable growth rate in the forecasted period, primarily in palliative care for bone metastases as a readily available and economical option for systemic radiotherapy. This radiopharmaceutical is routinely used for pain relief for patients with metastatic prostate and breast cancer, and the continued use of samarium-153 has developed off-labeled use and supportive care toward incremental use in oncology clinics.
Hospitals or Outpatient Centers: Who’s Leading Radiotherapy Delivery?
The hospitals segment led the systemic radiotherapy market due to their extensive oncology infrastructure, including PET/SPECT imaging, radiopharmacy labs, and multi-disciplinary tumor boards, which allows for comprehensive integrated administration of systemic radiotherapies such as I-131 and Samarium-153. Oncology centers within hospitals tend to have established workflows, and reimbursement timing is clear and concise, with existing pathways making them generally easier to work with than standalone or smaller clinical sites.
The independent radiotherapy centers segment is expected to grow at the fastest rate in the forecasted period. Overall, this growth in the delivery of outpatient independent radiotherapy centers stems from the decentralization of care, cost competitiveness, and patient preference for point-of-care services outside of large hospital environments. Independent radiotherapy centers frequently enter partnership agreements with academic medical centers that allow access to systemic radiotherapy protocols and develop a radiopharmacy capability.
Why Is Solid Tumor Treatment Emerging in Radiotherapy Applications?
The hematological malignancies segment captured a significant portion of the What Are the Opportunities in the systemic radiotherapy market? In 2024. This is because systemic radiotherapy, like I-131, supports the treatment and responds well with blood cancers such as leukemia and lymphoma, which makes it the most common application area in the market.
The solid tumors segment is projected to expand rapidly in the market in the coming years. This rapid growth rate is due to newer radiopharmaceuticals like the lutetium-177 agents, which have reached the late-stage clinical trials and have been approved for the treatment of liver, prostate, and thyroid cancers, with their application widening outside of blood cancers.
Mechanism of Action Insights
The direct cell targeting segment dominated the market because of its capability of delivering radioactive agents directly to the cancer cells and providing accurate treatment with a lot fewer side effects than other treatments. Thus, direct cell targeting is preferred in most therapies due to its proven reliability in the treatment process.
The targeted gene delivery segment is expected to grow at the fastest rate in the market during the forecast period of 2025 to 2034, as this method of treatment allows radiation therapy to reach targeted genes in the tumors more safely, further improving outcomes in trials, which has boosted its adoption rate in clinics and research centers.
What’s Driving the Shift from Palliative to Curative Radiotherapy?
The palliative care segment captured a significant portion of the market in 2024. This is because palliative care is one of the main purposes, as treatment such as the Samarium-153 is commonly used to relieve pain, and these therapies offer quick relief, thus improving the quality of life.
The curing cancer segment will gain a significant share of the systemic radiotherapy market over the studied period of 2025 to 2034 because more systemic therapies were approved in 2024 and expanded for the treatment of metastatic prostate cancer, and will expand beyond just pain relief.
North America
North America led the global systemic radiotherapy market in 2024 due to its high-quality healthcare delivery and the role of nuclear medicine products. North America has an established nuclear medicine market and well-developed radiopharmaceutical capabilities and application services, with the U.S. leading in clinical application of systemically administered radiotherapy agents such as lutetium-177 and iodine-131. The U.S. also has favorable FDA approvals, and reimbursement will facilitate patient access to radioisotopes and radiopharmaceutical therapies. North America is home to established pharmaceutical organizations that have design expertise; for example, Curium, Lantheus, and Cardinal Health have provided a robust supply chain for radioisotopes and the provision of overall theranostic care to deliver precision radiation therapy. Given the need to prevent further conditioning by the U.S. clinical research and healthcare in developing evidence-based treatment interventions for the rising incidence of metastatic cancers, as well as the trend towards more personalized medicine, there is further demand for the treatment of cancer with radiopharmaceuticals and radioisotopes.
Furthermore, several major research centers/hospitals are also integrating artificial intelligence-based dosimetry platforms that will provide increased precision therapeutic delivery. There will be several opportunities to advance the field, both regionally and globally, by expanding indications for the use of already approved agents, developing advanced digital twin modeling for predicting the course of therapy, and a greater demand for outpatient radiopharmaceutical therapy centers. In addition, major investments by government agencies in the production of isotopes, new funding declarations as part of the COVID-19 process, and the realization of greater collaborations with academia and the industries will further foster and strengthen North America's position as a leader in the systemic radiotherapy space.
Asia-Pacific
The Asia-Pacific is anticipated to be the fastest-growing in the systemic radiotherapy market in the forecasted period. Reasons for growth in the region stem from rapidly increasing prevalence of cancer, increasing health care investments, government-supported and rapid modernization of nuclear medicine infrastructure, and emerging markets for medical tourism. China, India, South Korea, Australia, and others have committed to funding radiopharmaceutical production facilities and are making significant investments in expanding access to radiotherapy services beyond urban centers.
Countries are developing government-supported initiatives to fund diagnostic services to enable early detection and care, as well as personalized treatments, and therefore, demand for systemic therapy clinical trials, such as 131-I MIBG and Lu-177 DOTATATE, is expanding rapidly. Furthermore, rising medical tourism and increasing public knowledge of the most advanced cancer treatments in the Asia-Pacific region are influencing the uptake of radiopharmaceuticals prescribed in systemic therapies. Multinational companies are increasingly entering the Asia-Pacific market through collaborations with local distributors and/or through local partnerships with academic programs.
The systemic radiotherapy market is highly competitive. There are a lot of international brands and companies in the systematic radiotherapy market, but some of the prominent players in the market include:
Varian Medical Systems operates in over seventy countries and sells radiotherapy and radiosurgery equipment (TrueBeam, Edge, Halcyon, ProBeam), oncology software, and brachytherapy equipment. Varian is well recognized for its automation innovations in LINAC, adaptive therapy driven by AI, and its Ethos System.
Elekta is a Swedish medical-technology company that operates in over 120 countries and sells precision radiotherapy solutions, including MR-Linac (Unity), Gamma Knife, Versa HD, Evo, Monaco planning software, MOSAIQ workflow systems, and brachytherapy products.
Accuray operates and sells advanced radiation therapy (in 50 countries globally), including CyberKnife, TomoTherapy/Radixact platforms, and Accuray Precision treatment planning and data-management tools for stereotactic radiosurgery and SBRT.
| Regions | Shares (%) |
| North America | 40% |
| Asia Pacific | 30% |
| Europe | 20% |
| LAMEA | 10% |
| Segments | Shares (%) |
| Hematological Malignancies | 45% |
| Solid Tumors | 55% |
| Segments | Shares (%) |
| Hospitals | 50% |
| Research Institutes | 20% |
| Outpatient Clinics | 20% |
| Diagnostic Centers | 10% |
| Segments | Shares (%) |
| Direct Cell Targeting | 40% |
| Targeted Gene Delivery | 35% |
| Combination Therapies | 25% |
| Segments | Shares (%) |
| Palliative Care | 30% |
| Curing Cancer | 35% |
| Adjuvant Treatment | 25% |
| Salvage Therapy | 10% |
Published by Kesiya Chacko
| By_Application_Area | 2024 | 2025 | 2026 | 2027 | 2028 | 2029 | 2030 | 2031 | 2032 | 2033 | 2034 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hematological Malignancies | 2.35 | 2.52 | 2.70 | 2.90 | 3.11 | 3.34 | 3.58 | 3.85 | 4.13 | 4.43 | 4.75 |
| Solid Tumors | 2.87 | 3.10 | 3.34 | 3.60 | 3.88 | 4.19 | 4.52 | 4.87 | 5.25 | 5.66 | 6.11 |
| By_End_User | 2024 | 2025 | 2026 | 2027 | 2028 | 2029 | 2030 | 2031 | 2032 | 2033 | 2034 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospitals | 2.61 | 2.81 | 3.02 | 3.26 | 3.50 | 3.77 | 4.06 | 4.37 | 4.70 | 5.06 | 5.45 |
| Research Institutes | 1.04 | 1.13 | 1.21 | 1.31 | 1.41 | 1.52 | 1.64 | 1.77 | 1.91 | 2.05 | 2.22 |
| Outpatient Clinics | 1.04 | 1.13 | 1.21 | 1.31 | 1.41 | 1.52 | 1.64 | 1.77 | 1.91 | 2.06 | 2.22 |
| Diagnostic Centers | 0.52 | 0.56 | 0.59 | 0.63 | 0.67 | 0.71 | 0.76 | 0.81 | 0.86 | 0.92 | 0.97 |
| By_Region | 2024 | 2025 | 2026 | 2027 | 2028 | 2029 | 2030 | 2031 | 2032 | 2033 | 2034 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| North America | 2.09 | 2.25 | 2.42 | 2.61 | 2.82 | 3.03 | 3.27 | 3.52 | 3.80 | 4.09 | 4.41 |
| Asia Pacific | 1.57 | 1.68 | 1.80 | 1.93 | 2.07 | 2.21 | 2.37 | 2.54 | 2.72 | 2.92 | 3.12 |
| Europe | 1.04 | 1.13 | 1.22 | 1.31 | 1.42 | 1.53 | 1.66 | 1.79 | 1.93 | 2.09 | 2.25 |
| LAMEA | 0.52 | 0.56 | 0.60 | 0.65 | 0.70 | 0.75 | 0.80 | 0.87 | 0.93 | 1.00 | 1.07 |
Last Updated: 01 Aug 2025
Source: Statifacts
| Subsegment | 2024 | 2025 | 2026 | 2027 | 2028 | 2029 | 2030 | 2031 | 2032 | 2033 | 2034 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hematological Malignancies | 2.35 | 2.52 | 2.70 | 2.90 | 3.11 | 3.34 | 3.58 | 3.85 | 4.13 | 4.43 | 4.75 |
| Solid Tumors | 2.87 | 3.10 | 3.34 | 3.60 | 3.88 | 4.19 | 4.52 | 4.87 | 5.25 | 5.66 | 6.11 |
| Subsegment | 2024 | 2025 | 2026 | 2027 | 2028 | 2029 | 2030 | 2031 | 2032 | 2033 | 2034 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospitals | 2.61 | 2.81 | 3.02 | 3.26 | 3.50 | 3.77 | 4.06 | 4.37 | 4.70 | 5.06 | 5.45 |
| Research Institutes | 1.04 | 1.13 | 1.21 | 1.31 | 1.41 | 1.52 | 1.64 | 1.77 | 1.91 | 2.05 | 2.22 |
| Outpatient Clinics | 1.04 | 1.13 | 1.21 | 1.31 | 1.41 | 1.52 | 1.64 | 1.77 | 1.91 | 2.06 | 2.22 |
| Diagnostic Centers | 0.52 | 0.56 | 0.59 | 0.63 | 0.67 | 0.71 | 0.76 | 0.81 | 0.86 | 0.92 | 0.97 |
| Subsegment | 2024 | 2025 | 2026 | 2027 | 2028 | 2029 | 2030 | 2031 | 2032 | 2033 | 2034 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| North America | 2.09 | 2.25 | 2.42 | 2.61 | 2.82 | 3.03 | 3.27 | 3.52 | 3.80 | 4.09 | 4.41 |
| Asia Pacific | 1.57 | 1.68 | 1.80 | 1.93 | 2.07 | 2.21 | 2.37 | 2.54 | 2.72 | 2.92 | 3.12 |
| Europe | 1.04 | 1.13 | 1.22 | 1.31 | 1.42 | 1.53 | 1.66 | 1.79 | 1.93 | 2.09 | 2.25 |
| LAMEA | 0.52 | 0.56 | 0.60 | 0.65 | 0.70 | 0.75 | 0.80 | 0.87 | 0.93 | 1.00 | 1.07 |
Systemic radiotherapy involves administering radioactive agents, via intravenous, oral, or instillation routes, that home in on specific tissues or tumors throughout the body. Unlike external or internal beam methods, these therapies circulate and deliver targeted radiation internally to metastatic or diffuse disease sites.
Growth is fueled by expanding use in metastatic cancers, especially neuroendocrine tumors and prostate cancer, alongside advances in targeted radioconjugates. Biotech investments and acquisitions are strengthening research and development and clinical pipelines.
Radioligand therapies like Pluvicto (Lu 177 PSMA) for metastatic prostate cancer and Lutathera (Lu 177 dotatate) for neuroendocrine tumors are established offerings. Major players include Novartis, AstraZeneca (via Fusion acquisition), IBA, Eckert & Ziegler, and Nordion.
North America, led by the U.S., remains the epicenter due to regulatory approvals, manufacturing capacity, and clinical infrastructure. Emerging adoption is strongest in Europe and Asia Pacific, where investment in radiotheranostics is rapidly expanding.
Challenges include complex isotope production, short radionuclide half-lives, high treatment costs, and regulatory hurdles. But innovation opportunities are gaining momentum in alpha emitter therapies, personalized theranostics, AI assisted targeting, and tighter integration of diagnostics with therapy.
To get full access to our Market Insights, you need a Professional Account or a Business Suite.
You will receive an email from our Business Development Manager. Please be sure to check your SPAM/JUNK folder too.
You will receive an email from our Business Development Manager. Please be sure to check your SPAM/JUNK folder too.

Our customers work more efficiently and benefit from